HUMAN REPRODUCTION
As you are aware, humans are sexually reproducing and viviparous.
The reproductive events in humans include
- formation of gametes (gametogenesis), i.e., sperms in males and ovum in females,
- transfer of sperms into the female genital tract (insemination) and
- fusion of male and female gametes (fertilisation) leading to formation of zygote.
- This is followed by formation and development of blastocyst and its attachment to the uterine wall (implantation),
- embryonic development (gestation) and
- delivery of the baby (parturition).
- There are remarkable differences between the reproductive events in the male and in the female, for example, sperm formation continues even in old men, but formation of ovum ceases in women around the age of fifty years.
3.1 THE MALE REPRODUCTIVE SYSTEM
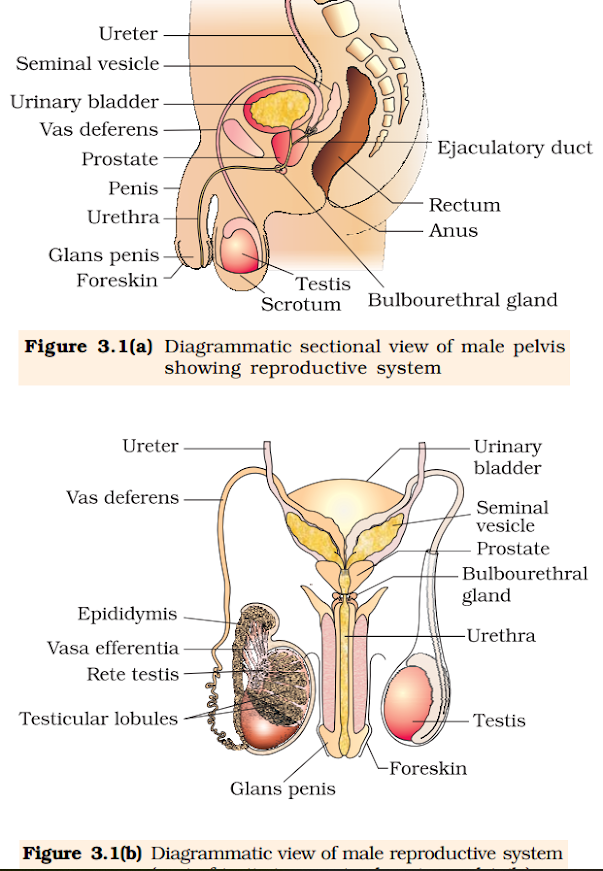
The male reproductive system is located in the pelvis region (Figure 3.1a).
It includes a pair of testes along-with accessory ducts, glands and the external genitalia.
- The testes are situated outside the abdominal cavity within a pouch called scrotum.
- The scrotum helps in maintaining the low temperature of the testes (2–2.5o C lower than the normal internal body temperature) necessary for spermatogenesis.
- In adults, each testis is oval in shape, with a length of about 4 to 5 cm and a width of about 2 to 3 cm.
- The testis is covered by a dense covering. Each testis has about 250 compartments called testicular lobules (Figure 3.1b).
- Each lobule contains one to three highly coiled seminiferous tubules in which sperms are produced.
- Each seminiferous tubule is lined on its inside by two types of cells called male germ cells (spermatogonia) and Sertoli cells (Figure 3.2 ).
- The male germ cells undergo meiotic divisions finally leading to sperm formation, while Sertoli cells provide nutrition to the germ cells.
- The regions outside the seminiferous tubules called interstitial spaces, contain small blood vessels and interstitial cells or Leydig cells (Figure 3.2).
- Leydig cells synthesise and secrete testicular hormones called androgens.
- Other immunologically competent cells are also present.
The male sex accessory ducts include rete testis, vasa efferentia, epididymis and vas deferens (Figure 3.1b).
- The seminiferous tubules of the testis open into the vasa efferentia through rete testis.
- The vasa efferentia leave the testis and open into epididymis located along the posterior surface of each testis.
- The epididymis leads to vas deferens that ascends to the abdomen and loops over the urinary bladder.
- It (vas deferens) receives a duct from seminal vesicle and opens into urethra as the ejaculatory duct (Figure 3.1a).
- These ducts store and transport the sperms from the testis to the outside through urethra.
- The urethra originates from the urinary bladder and extends through the penis to its external opening called urethral meatus.
- It is made up of special tissue that helps in erection of the penis to facilitate insemination.
- The enlarged end of penis called the glans penis is covered by a loose fold of skin called foreskin.
- paired seminal vesicles, a prostate and paired bulbourethral glands.
- Secretions of these glands constitute the seminal plasma which is rich in fructose, calcium and certain enzymes.
- The secretions of bulbourethral glands also helps in the lubrication of the penis.
- The female reproductive system consists of
- a pair of ovaries along with
- a pair of oviducts,
- uterus,
- cervix,
- vagina and
- the external genitalia located in pelvic region (Figure 3.3a).
- Each fallopian tube is about 10-12 cm long and extends from the periphery of each ovary to the uterus (Figure 3.3b), the part closer to the ovary is the funnel-shaped infundibulum.
- The edges of the infundibulum possess finger-like projections called fimbriae, which help in collection of the ovum after ovulation.
- The infundibulum leads to a wider part of the oviduct called ampulla. The last part of the oviduct, isthmus has a narrow lumen and it joins the uterus.
- The shape of the uterus is like an inverted pear. It is supported by ligaments attached to the pelvic wall.
- The uterus opens into vagina through a narrow cervix.
- The cavity of the cervix is called cervical canal (Figure 3.3b) which along with vagina forms the birth canal.
- The wall of the uterus has three layers of tissue.
- The external thin membranous perimetrium, middle thick layer of smooth muscle, myometrium and inner glandular layer called endometrium that lines the uterine cavity.
- The endometrium undergoes cyclical changes during menstrual cycle while the myometrium exhibits strong contraction during delivery of the baby.
- Mons pubis, labia majora, labia minora, hymen and clitoris (Figure 3.3a).
- Mons pubis is a cushion of fatty tissue covered by skin and pubic hair.
- The labia majora are fleshy folds of tissue, which extend down from the mons pubis and surround the vaginal opening.
- The labia minora are paired folds of tissue under the labia majora.
- The opening of the vagina is often covered partially by a membrane called hymen.
- The clitoris is a tiny finger-like structure which lies at the upper junction of the two labia minora above the urethral opening.
- The hymen is often torn during the first coitus (intercourse).
- These parts of the system along with a pair of the mammary glands are integrated structurally and functionally to support the processes of ovulation, fertilisation, pregnancy, birth and child care.
- The ovaries are located one on each side of the lower abdomen (Figure 3.3b).
- Each ovary is about 2 to 4 cm in length and is connected to the pelvic wall and uterus by ligaments.
- Each ovary is covered by a thin epithelium which encloses the ovarian stroma. The stroma is divided into two zones – a peripheral cortex and an inner medulla.
- A functional mammary gland is characteristic of all female mammals.
The mammary glands are paired structures (breasts) that contain glandular tissue and variable amount of fat.
- The glandular tissue of each breast is divided into 15-20 mammary lobes containing clusters of cells called alveoli (Figure 3.4).
- The cells of alveoli secrete milk, which is stored in the cavities (lumens) of alveoli.
- The alveoli open into mammary tubules.
- The tubules of each lobe join to form a mammary duct. Several mammary ducts join to form a wider mammary ampulla which is connected to lactiferous duct through which milk is sucked out.
- The primary sex organs – the testis in the males and the ovaries in the females – produce gametes, i.e, sperms and ovum, respectively, by the process called gametogenesis.
- In testis, the immature male germ cells (spermatogonia) produce sperms by spermatogenesis that begins at puberty.
- The spermatogonia (sing. spermatogonium) present on the inside wall of seminiferous tubules multiply by mitotic division and increase in numbers.
- Each spermatogonium is diploid and contains 46 chromosomes. Some of the spermatogonia called primary spermatocytes periodically undergo meiosis.
- A primary spermatocyte completes the first meiotic division (reduction division) leading to formation of two equal, haploid cells called secondary spermatocytes, which have only 23 chromosomes each.
- The secondary spermatocytes undergo the second meiotic division to produce four equal, haploid spermatids (Figure 3.5).
- What would be the number of chromosome in the spermatids?
- The spermatids are transformed into spermatozoa (sperms) by the process called spermiogenesis.
- After spermiogenesis, sperm heads become embedded in the Sertoli cells, and are finally released from the seminiferous tubules by the process called spermiation.
- Spermatogenesis starts at the age of puberty due to significant increase in the secretion of gonadotropin releasing hormone (GnRH).
- This, if you recall, is a hypothalamic hormone.
- The increased levels of GnRH then acts at the anterior pituitary gland and stimulates secretion of two gonadotropins – luteinising hormone (LH) and follicle stimulating hormone (FSH).
- LH acts at the Leydig cells and stimulates synthesis and secretion of androgens.
- Androgens, in turn, stimulate the process of spermatogenesis.
- FSH acts on the Sertoli cells and stimulates secretion of some factors which help in the process of spermiogenesis.
- It is a microscopic structure composed of a head, neck, a middle piece and a tail (Figure 3.6).
- A plasma membrane envelops the whole body of sperm.
- The sperm head contains an elongated haploid nucleus, the anterior portion of which is covered by a cap-like structure, acrosome.
- The acrosome is filled with enzymes that help fertilisation of the ovum.
- The middle piece possesses numerous mitochondria, which produce energy for the movement of tail that facilitate sperm motility essential for fertilisation.
- The human male ejaculates about 200 to 300 million sperms during a coitus of which, for normal fertility, at least 60 per cent sperms must have normal shape and size and for at least 40 per cent of them must show vigorous motility.
- Sperms released from the seminiferous tubules, are transported by the accessory ducts.
- Secretions of epididymis, vas deferens, seminal vesicle and prostate are essential for maturation and motility of sperms.
- The seminal plasma along with the sperms constitute the semen.
- The functions of male sex accessory ducts and glands are maintained by the testicular hormones (androgens).
- The process of formation of a mature female gamete is called oogenesis which is markedly different from spermatogenesis.
- Oogenesis is initiated during the embryonic development stage when a couple of million gamete mother cells (oogonia) are formed within each fetal ovary; no more oogonia are formed and added after birth.
- These cells start division and enter into prophase-I of the meiotic division and get temporarily arrested at that stage, called primary oocytes.
- Each primary oocyte then gets surrounded by a layer of granulosa cells and then called the primary follicle (Figure 3.7).
- A large number of these follicles degenerate (follicular atresia) during the phase from birth to puberty. Therefore, at puberty only 60,000-80,000 primary follicles are left in each ovary.
- The primary follicles get surrounded by more layers of granulosa cells and a new theca and called secondary follicles.
- The secondary follicle soon transforms into a tertiary follicle which is characterised by a fluid filled cavity called antrum.
- The theca layer is organised into an inner theca interna and an outer theca externa.
- It is important to draw your attention that it is at this stage that the primary oocyte within the tertiary follicle grows in size and completes its first meiotic division.
- It is an unequal division resulting in the formation of a large haploid secondary oocyte and a tiny first polar body (Figure 3.8b).
- The secondary oocyte retains bulk of the nutrient rich cytoplasm of the primary oocyte. Can you think of any advantage for this?
- Does the first polar body born out of first meiotic division divide further or degenerate? At present we are not very certain about this.
- The tertiary follicle further changes into the mature follicle or Graafian follicle (Figure 3.7). The secondary oocyte forms a new membrane called zona pellucida surrounding it.
- The Graafian follicle now ruptures to release the secondary oocyte (ovum) from the ovary by the process called ovulation.
- Can you identify major differences between spermatogenesis and oogenesis?
- A diagrammatic representation of
spermatogenesis and oogenesis is given below (Figure 3.8).






Comments
Post a Comment